UNIVERSITY SARCOMA NETWORK
University network for the orthopaedic treatment and research of sarcomas and other tumours
The university hospitals of Balgrist in Zurich, Inselspital in Bern, University Children's Hospital in Basel as well as HUG in Geneva and CHUV in Lausanne have joined together to form the “University Sarcoma Network”. Each of the hospitals operates its own highly specialised sarcoma centre and treats patients with musculoskeletal tumours (sarcomas). The network promotes the exchange of information and inter-university cooperation between the sarcoma centres.
Highly specialised medicine in the treatment of sarcomas
Bone and soft-tissue tumours are extremely complex diseases that present a particular challenge because of their rarity. The treatment of sarcomas involves interdisciplinary input from several specialties (e.g. tumour surgery, oncology, radiology, etc.). Thanks to their high degree of specialisation and evidence-based research, the university sarcoma centres can offer the best-possible treatment to patients with bone and soft-tissue tumours.
A second opinion for the patient
When faced with a serious malignant disease, patients need assurance as quickly as possible. For this reason, patients can ask the University Sarcoma Network for a qualified independent second opinion regarding the diagnosis and treatment of their cancer. Leading experts assess whether the proposed therapy corresponds to the latest medical thinking.
Case discussion in the sarcoma network
The surgical treatment of sarcomas often requires difficult decisions. Tumour surgeons therefore regularly discuss complex cases at case conferences. The experts involved deliberate the possible therapeutic options and make decisions tailored to the individual patient. Thanks to the sarcoma network, affected patients benefit from the surgical expertise of all the sarcoma centres and receive continuous treatment of the highest quality.
Frequently asked questions
What are bone and soft-tissue tumours?
As with the internal organs, tumours may develop in bones and soft tissues. They are most commonly found in the arms, legs and pelvis, and are often located close to a joint. Bone and soft-tissue tumours are classified as benign and malignant (cancer). Malignant tumours carry the risk of spreading to other parts of the body and forming new lesions, especially in the small blood vessels in the lungs.
What is a sarcoma?
Sarcoma is the technical term for malignant tumours (cancers) that arise directly in bone or soft tissues (fatty tissue, muscles, connective tissue, and nerve tissue). If cancer spreads to the bones from other organs (prostate, breast, lungs, thyroid gland, etc.), we call these lesions secondaries or metastases.
What sort of tumours are there?
The three most common cancers in bone are osteosarcomas, chondrosarcomas and Ewing’s sarcomas. Liposarcoma (in fatty tissue) is the commonest malignant tumour found in soft tissue. Each type of tumour requires individual treatment.
What causes bone and soft-tissue cancer?
Compared with other types of cancer, bone and soft-tissue cancers are very rare. No clear cause has yet been discovered. Lifestyle and diet in particular do not seem to affect their development.
Work-up and diagnosis
If a bone or soft-tissue tumour is suspected, the patient can contact one of the five university hospitals that make up the University Sarcoma Network. The advantage is that all the institutes have their own certified sarcoma centre. Irrespective of where they live, patients can benefit from the expertise of sarcoma specialists. Each sarcoma centre will carry out their own in-depth investigations and diagnostic imaging whenever there is a firm suspicion of cancer. Patients are invited to attend the outpatient clinic. A tissue specimen (biopsy) is often needed to confirm the diagnosis.
What is a biopsy?
A biopsy consists of taking a small piece of tissue from the tumour and examining it under the microscope. The biopsy tells us what type of tumour is present and how aggressively it is growing. Biopsies are performed as gently as possible, using minimally invasive techniques. A fine needle is inserted into the tumour under CT or ultrasound guidance. This procedure can be done as an outpatient and an anaesthetist will help to ensure that it is as comfortable as possible for the patient.
What does the diagnosis mean to the person concerned?
A diagnosis of cancer places a considerable burden on affected individuals and their relatives. The choice of treatment and the corresponding therapeutic goal depends on the results of diagnostic investigations. Time spent waiting is usually filled with anxiety and uncertainty about the future. The results are assessed by specialists from all the relevant disciplines to recommend optimal treatment and implement it as quickly as possible. All treatment – whether surgery, chemotherapy or radiotherapy – is basically associated with physical restrictions and psychological stress. Even so, the treatment phase is often found to be less stressful than the time before the start of treatment. Once treatment is complete, some form of regular cancer aftercare is usually necessary to identify any recurrence promptly.
Surgery
Surgery on a tumour is always a team affair for tumour and joint specialists. The top priority in an operation is to remove the tumour correctly and completely; this is the basis of successful treatment. Thanks to huge advances in the surgical resection of bone and soft-tissue tumours, amputations are now needed only in exceptional cases – which means that the patient can recover the use of an affected joint as far as possible.
Radiotherapy (irradiation)
Besides surgery and chemotherapy, radiotherapy is of great value in the treatment of sarcomas. The sarcoma is irradiated with high-energy ionising rays. The aim is to disrupt the DNA of the tumour cells and prevent further growth of the tumour. The technique employed may be through the skin (external) with a linear accelerator or from the inside (internal) by brachytherapy. In addition, the surgeon may work with the radiotherapist to apply intraoperative radiotherapy (IORT) by irradiating the tumour bed immediately after the tumour has been removed. State-of-the-art equipment and scientifically tested and accepted therapeutic options are available for the treatment of sarcomas. The regular exchange of information with the other institutes means that we can ensure comprehensive high-quality treatment and care.
Chemotherapy
Chemotherapy involves treating the sarcoma with medication. Medicines can be given before an operation (neoadjuvant), after an operation (adjuvant), or to relieve symptoms (palliative care). Chemotherapy prior to surgery aims to reduce the size of the tumour, making the operation easier and subsequent radiotherapy more effective. When given after the removal of the tumour, chemotherapy aims to eliminate any remaining cancer that is not visible to the naked eye, and it may also help to reduce the risk of recurrence. Chemotherapy uses substances targeted at specific cancer cells, in order to kill them or inhibit their growth. The particular medicines used depend on the nature of the sarcoma.
Research
Due to the rarity of sarcomas, clinicians also work closely together in research.
Clinical research
A particular focus of clinical research is the mutual development and evaluation of new surgical techniques, as well as measuring the quality of life during and after treatment. Innovative clinical studies are being carried out, in which patients become involved after in-depth discussion. In this way, they have early access to new therapy and medication.
Basic scientific research
Various scientific research projects are underway:
- Liquid biopsies (isolating and testing circulating cancer cells in the blood)
- Exchange of tissue specimens (tissues from the biobanks of the university hospitals are being combined to increase the quality and effectiveness of studies)
- More accurate imaging procedures
- Surgical techniques (computer-planned tumour resection by means of 3D implants)
- Personalised treatment (with tumours of the musculoskeletal system, each patient should be offered individual long-term targeted therapy according to the properties of the cancer cells and DNA changes)
Vocational training
In order to ensure first-class treatment for the patient, the Sarcoma Network takes the responsibilities of professional tumour surgery very seriously and focusses strongly on the vocational training of orthopaedic surgeons. Surgeons with a special interest in tumour surgery are particularly encouraged.
Members of the Sarcoma Centres
Your contacts in the Sarcoma Centres in Switzerland

Prof. Dr. med. Mazda Farshad, MPH
Medical Director, Chief of Orthopaedics

PD Dr. med. Daniel Andreas Müller
Head of Tumour Surgery

Dr. med. Dominik Kaiser
Consultant, Tumour Surgery
Sarcoma Center Zurich
tumoren@sekretariat.ch
Phone: +41 44 386 30 95

Prof. Dr. med. Klaus Siebenrock
Medical Director, Chief of Orthopaedic and Trauma Surgery

Prof. Dr. med. Dr. phil. nat. Frank Klenke
Head of Sarcoma Centre
Senior Consultant, Orthopaedic and Trauma Surgery
Sarcoma Centre Inselspital
sarkomzentrum@insel.ch
Phone: +41 31 632 58 46

Prof. Didier Hannouche
Head of Orthopaedic and Trauma Surgery
didier.hannouche@hcuge.ch
Phone: +41 22 372 78 02

Prof. Alain Farron
Professor, Head of Department
alain.farron@chuv.ch
Phone: +41 21 314 94 03

Dr. Stephane Cherix
Consultant
Mobile: +41 79 556 79 52

Prof. Dr. med. Andreas H. Krieg
Senior Physician Orthopedics
Co-Head of the Center for Bone and Soft Tissue Tumors (Sarcoma Center Basel)
andreas.krieg@ukbb.ch
Tel: +41 61 704 18 06 / 04

Prof. Dr. med. Andreas Marc Müller
Head physician a.i. / Team leader
Shoulder/elbow orthopedics
Orthopedics and Traumatology
Dr. med. Thierry Fleury
Consultant Orthopedics
Bone and Soft Tissue Tumor Center
of the University of Basel (KWUB)
kwub@ukbb.ch
Tel: +41 61 704 28 47

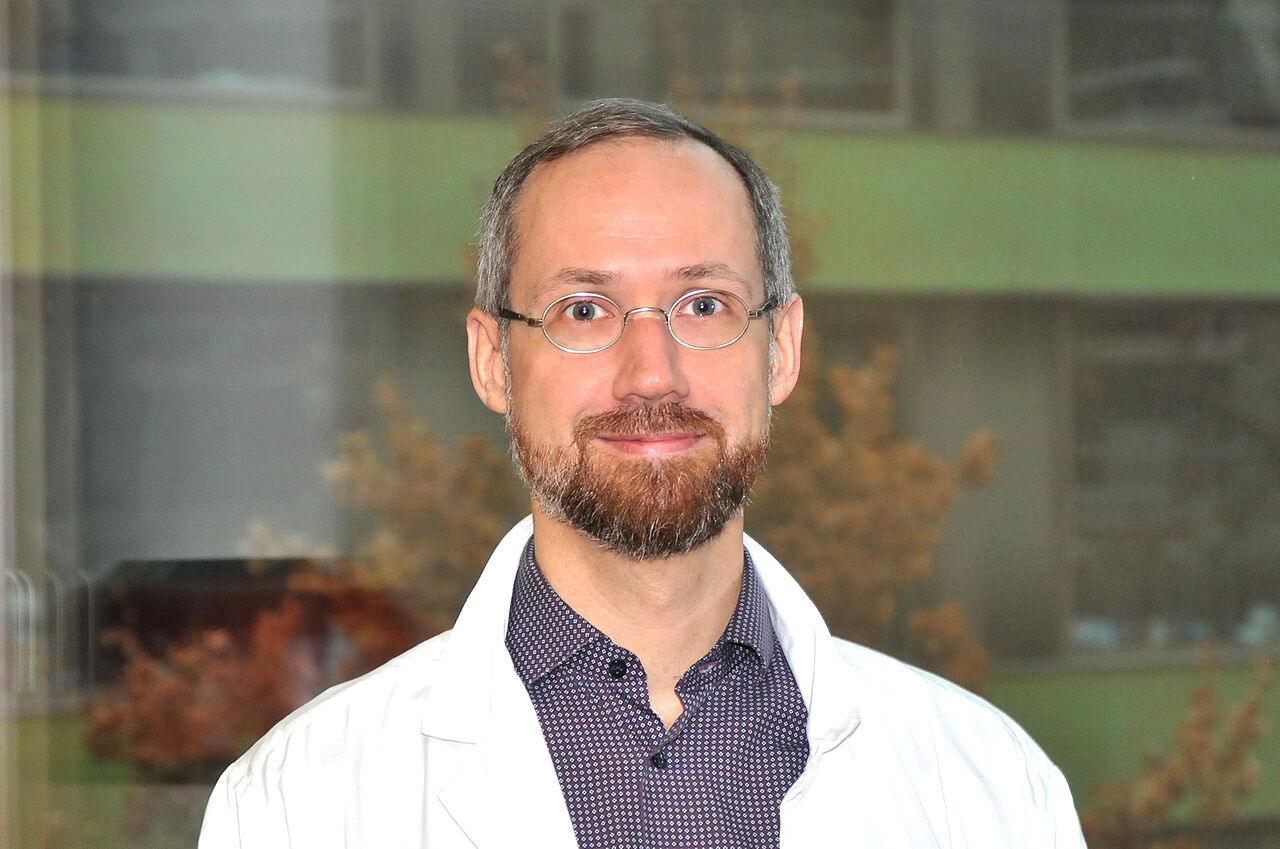
Prof. Dr. med. Daniel Baumhoer
Deputy Chief Physician Pathology
Bone Tumor Reference Center Pathology / USB Basel Schönbeinstrasse 40
CH-4031 Basel
Tel.: +41-61-2652878
ktrz@usb.ch